Diabetic eye diseases encompass a group of eye conditions that affect those with diabetes, including diabetic retinopathy, diabetic macular edema, cataracts, and glaucoma. These conditions can lead to severe vision loss or even blindness if not managed properly. The root of these complications lies in the damage to the tiny blood vessels in the retina, caused by high blood glucose levels. Regular eye exams play a crucial role in early detection and management, helping to prevent irreversible damage to your eyes.
It’s essential for individuals with diabetes to understand the risks and signs of diabetic eye diseases. The American Diabetes Association highlights that diabetes doubles the risk for diabetic eye disease, making regular monitoring and control of blood glucose levels imperative. Symptoms like blurred vision or the appearance of floaters may signal the onset of these conditions. Early intervention through comprehensive eye care and management of diabetes can significantly protect your vision and reduce the risk of vision loss and blindness.
Understanding Diabetic Eye Disease
Understanding diabetic eye disease begins with recognizing how diabetes affects the eyes. High blood glucose levels can damage the tiny blood vessels in the retina, leading to conditions like diabetic retinopathy and diabetic macular edema. These eye diseases threaten sight and can lead to vision loss if not addressed in a timely manner. The National Eye Institute underscores the importance of early detection and management of these conditions. Regular eye exams allow for prompt diagnosis and treatment, offering the best chance to protect your vision from the serious effects of diabetes.
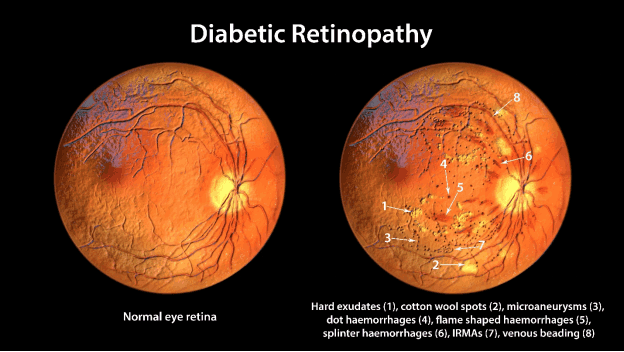
Diabetic Retinopathy: The Leading Concern
Diabetic retinopathy stands as the most significant eye health challenge for individuals with diabetes. It occurs when high glucose levels cause damage to the blood vessels in the retina, the light-sensitive layer of tissue at the back of the eye. These damaged blood vessels can leak, swell, or develop abnormal new blood vessels, leading to vision problems. Without timely treatment, diabetic retinopathy can progress, potentially resulting in blindness. Therefore, understanding and early management of this condition are crucial for preserving eye health.
Diabetic Macular Edema: A Close Second
Following closely behind diabetic retinopathy in terms of risk is diabetic macular edema (DME). DME arises as a complication of diabetic retinopathy, characterized by the accumulation of fluid in the macula—part of the retina that controls detailed vision. Signs of diabetic retinopathy like blurred vision can indicate the onset of DME. This condition can severely impair the ability to read, drive, and perform other activities that require sharp vision. Prompt detection and treatment are key to managing DME effectively.
Symptoms of Diabetic Eye Disease: What to Watch For
Symptoms of diabetic eye disease can vary but often include blurry or wavy vision, flashes of light, impaired color vision, and the appearance of spots or dark strings floating in the vision. These symptoms indicate the need for an immediate consultation with an eye doctor. Early detection of symptoms and timely intervention can significantly reduce the risk of severe vision loss. Individuals experiencing these symptoms should not delay in seeking professional advice to protect their sight.
The Spectrum of Eye Problems in Diabetes
Diabetes can lead to a broad spectrum of eye problems, impacting vision in multiple ways. For women who develop gestational diabetes, there is an increased risk of developing vision complications. Yearly eye examinations are recommended to monitor changes. Diabetes affects the light-sensitive layer of the eye, causing vision to be blurry, which is a common complaint. This layer, crucial for capturing images and sending signals from the eye to the brain, is vulnerable to high blood sugar levels, underscoring the importance of managing diabetes effectively.
Beyond Retinopathy: Glaucoma and Cataracts
While diabetic retinopathy and macular edema are primary concerns, diabetes also increases the risk for other eye conditions such as glaucoma and cataracts. Glaucoma results from increased pressure in the eye that can damage the optic nerve, while cataracts are characterized by a cloudy lens that blurs vision. Both conditions can lead to significant vision loss if not treated. Regular eye exams are essential for early detection and management of these conditions, ensuring comprehensive eye care for individuals with diabetes.
Diagnosing and Treating Diabetic Eye Complications
Diagnosing and treating diabetic eye complications involves a combination of regular monitoring, managing blood glucose levels, and specific treatments depending on the condition. Blurry vision can often be the first sign of underlying issues, prompting further investigation. Growth of abnormal blood vessels, a symptom of advanced diabetic eye disease, may require interventions such as laser surgery or injections to preserve sight. Treatments are performed in a surgery center or hospital, emphasizing the importance of early detection through regular eye exams.
When to Consult an Eye Doctor for Diabetic Eye Disease
Consulting an eye doctor is crucial for anyone experiencing symptoms of diabetic eye disease or those managing diabetes. Effective management of diabetes, including controlling blood glucose, blood pressure, and cholesterol, can significantly reduce the risk of developing diabetic retinopathy. Regular consultations with eye care professionals help in monitoring eye health, making adjustments to diabetes management, and deciding on the best treatment options, including eye drops or more advanced procedures, to prevent vision loss.

Navigating the Diagnosis: Tests and Techniques
An eye doctor uses specialized tests and techniques, such as fluorescein angiography, to diagnose diabetic eye disease. This test involves injecting a dye into the bloodstream and taking images of the eye to observe the health of the blood vessels in the eye. It’s a crucial tool for detecting and assessing the extent of damage caused by diabetes.
The Role of Comprehensive Eye Exams
Comprehensive eye exams are pivotal in the early detection and management of diabetic eye disease. These exams allow eye care professionals to assess the health of the eye, detecting changes or damage caused by high blood glucose levels. Regular monitoring is essential for preventing progression and preserving vision, highlighting the importance of maintaining optimal blood glucose control as part of diabetes management.
Preventative Measures and Early Intervention
Preventative measures and early intervention are key strategies in minimizing the risk of diabetic eye disease. By managing blood glucose levels, individuals can protect their eye health and prevent the onset of vision-threatening conditions. Regular eye exams enable early detection and treatment, significantly reducing the risk of irreversible vision loss. Adopting a proactive approach to diabetes management and eye care can safeguard vision and enhance overall quality of life.
Risk Factors: Who is More Likely to Develop Diabetic Eye Disease?
Individuals with poorly controlled blood glucose levels are at greater risk of developing diabetic eye disease. Factors such as the duration of diabetes, high blood pressure, and high cholesterol also contribute to an increased risk. It’s essential for patients to understand these risks and work closely with their healthcare providers to manage their diabetes effectively, thereby reducing the likelihood of eye complications.
Proactive Steps to Shield Your Eyes from Diabetes
Taking proactive steps to shield your eyes from the impacts of diabetes involves diligent management of blood sugar levels and maintaining overall eye health. Strategies include adhering to a balanced diet, regular physical activity, and closely monitoring blood glucose levels. Such measures not only aid in controlling diabetes but also play a crucial role in preventing diabetic eye diseases. Engaging in regular eye exams allows for timely detection and management of any eye health issues, further protecting one’s vision.

The Importance of Regular Eye Examinations
Regular eye examinations are essential for anyone with diabetes, as they provide an opportunity for early detection and treatment of eye conditions before they progress to more serious stages. These exams are crucial for maintaining eye health and preventing diabetic eye disease, underscoring the importance of integrating eye care into the overall management of diabetes. By prioritizing eye health, individuals with diabetes can take significant steps toward preserving their vision and ensuring a higher quality of life.
When considering the best care for diabetic eye disease, the expertise of Dr. Claude Belgrave Jr. stands out. A distinguished Harvard Medical graduate (Top 10%) in Ophthalmology, Dr. Belgrave honed his expertise at Mount Sinai, one of the nation’s premier residency programs. With over 40 years of experience, he delivers exceptional eye care for both adults and children. Known for his precision, expertise, and genuine compassion, Dr. Belgrave has earned the trust of his patients—reflected in his stellar 4.8-star Google rating from 100+ glowing reviews. When it comes to your vision, don’t settle for anything less than extraordinary care. Offices are located in Suffolk, Va and Franklin, VA.
Managing Diabetes Effectively to Protect Vision
Keeping diabetes under control is vital for safeguarding your eyesight. This means regularly monitoring blood sugar levels to reduce the risk of developing diabetic retinopathy and other eye conditions. A balanced diet, regular physical activity, and adhering to medication regimens can significantly diminish the chances of severe vision loss. It’s also crucial to manage other risk factors, such as high blood pressure and cholesterol, which can exacerbate eye problems in those with 1 or type 2 diabetes.
Living with Diabetic Eye Disease
Diagnosis of a diabetic eye condition can initially be overwhelming, yet many individuals live fulfilling lives by adapting to their new reality. Adjusting daily routines and embracing assistive technologies can help maintain independence and quality of life. It’s essential to stay connected with healthcare providers to monitor the stages of the disease and prevent further vision impairment.
Support from family, friends, and diabetes care teams plays a significant role in navigating the challenges of diabetic eye disease. Emotional and practical support helps in coping with the adjustments and in making informed decisions about treatment options, including eye surgery if necessary.

Adjusting to Life with Vision Loss
Adjusting to vision loss requires time and patience. Simple modifications at home, such as using brighter lights and high-contrast items, can aid in daily activities. Learning new skills, like reading Braille or using voice-activated devices, also empowers individuals to continue enjoying books, music, and other hobbies.
Many find strength in community support groups where sharing experiences and tips with others facing similar challenges provides comfort and practical advice. Rehabilitation services offer training in mobility and activities of daily living, promoting independence despite vision changes.
Resources and Support for Individuals with Diabetic Eye Conditions
For those living with diabetic eye disease, a wealth of resources and support systems are available. National and local diabetes associations provide educational materials, workshops, and support groups. Healthcare teams, including ophthalmologists and diabetes educators, are essential for managing both diabetes and its ocular complications. They guide patients through the complexities of treatment for diabetic retinopathy, including comprehensive dilated eye exams and interventions to prevent blood vessels from growing abnormally.
The Future of Diabetic Eye Disease Management
Advancements in technology and medicine are continuously improving the outlook for diabetic eye disease management. Research is focused on developing more effective treatments to halt the progression of diabetic retinopathy and diabetic macular edema at various stages of the disease. With ongoing studies on gene therapy and innovative medications, the future holds promise for reducing the incidence of severe vision loss among diabetic patients.

The Latest Research on Diabetic Retinopathy and Diabetic Macular Edema
Recent studies have introduced breakthroughs in understanding and treating diabetic retinopathy and diabetic macular edema. Innovations in imaging technology allow for earlier detection and more precise monitoring of changes in the retina. Researchers are also exploring treatments that target the underlying causes of these conditions, including therapies designed to strengthen the blood-retinal barrier and prevent the leakage of the gel-like fluid that fills the eye.
Emerging Therapies and Future Prospects
The future of diabetic eye disease treatment is bright, with emerging therapies showing great potential. From injections that better control the formation of tiny bulges in blood vessels to cutting-edge eye surgery techniques for retinal detachment, patients have reasons to be optimistic. These advances could significantly reduce the risk and severity of vision loss, offering hope to millions affected by diabetes-induced eye conditions.
Conclusion: Empowering Yourself Against Diabetic Eye Disease
Understanding diabetic eye disease and taking proactive steps early on can make a significant difference in managing and preventing severe complications. Education, regular monitoring, and effective diabetes management are key components in protecting your vision.
The Importance of Knowledge and Early Action
Early detection and treatment are crucial in preventing vision loss from diabetic eye disease. Staying informed about your condition and maintaining regular check-ups can help catch and address issues before they escalate.
Staying Informed About Advances in Eye Care for Diabetics
Keeping up with the latest research and treatment options is essential for anyone affected by diabetic eye disease. Advances in care offer new possibilities for preserving and even improving vision, underscoring the importance of staying engaged with your eye care specialist.
Dr. Claude Belgrave Jr., a distinguished Harvard Medical graduate (Top 10%) in Ophthalmology, honed his expertise at Mount Sinai, one of the nation’s premier residency programs. With over 40 years of experience, he delivers exceptional eye care for both adults and children. Known for his precision, expertise, and genuine compassion, Dr. Belgrave has earned the trust of his patients—reflected in his stellar 4.8-star Google rating from 100+ glowing reviews. When it comes to your vision, don’t settle for anything less than extraordinary care. Offices are located in Suffolk, Va and Franklin, VA.
FAQ: Diabetic Eye Disease – Understanding and Managing Visual Complications
1. How does diabetes affect my vision?
Diabetes doubles the risk of developing eye diseases that can damage your vision, such as diabetic retinopathy or macular edema. High blood sugar can weaken blood vessels in the eye, causing them to swell, leak, or even bleed, leading to vision loss and blindness.
2. What is diabetic retinopathy?
Diabetic retinopathy is an eye disease that occurs when blood vessels may leak or become blocked, reducing oxygen supply to the retina. As it worsens, abnormal new blood vessels may grow, which can bleed into the gel-like fluid that fills the eye, resulting in vision will be blurry or severe visual impairment.
3. What are the stages of diabetic retinopathy?
The stages of diabetic retinopathy range from mild to severe:
- Mild & Moderate Nonproliferative: Early damage with tiny bulges in blood vessels.
- Severe Nonproliferative: Blocked blood vessels lead to decreased oxygen supply.
- Proliferative: Growth of abnormal new blood vessels, which can lead to serious complications like retinal detachment.
4. Can diabetes cause other eye diseases?
Yes, in addition to diabetic retinopathy, diabetes increases the risk of other eye diseases that can damage the optic nerve, such as glaucoma. It also makes people more likely to develop cataracts, which occurs when a cloudy lens in your eye affects vision clarity.
5. What is a detached retina, and how does it affect vision?
A detached retina happens when the retina pulls away from the back of the eye, cutting off communication between the eye to the brain. This can threaten your sight and lead to permanent blindness if not treated immediately.
6. How can I protect my vision if I have diabetes?
To protect your vision, you should focus on the management of your diabetes by maintaining average blood sugar, blood pressure and cholesterol within a healthy range. Regular eye exams can help detect issues early.
7. Why are eye exams important for people with diabetes?
Routine exams help diagnose eye problems before they progress. The American Academy of Ophthalmology and the National Institute of Health recommend annual check-ups. Pregnant women should schedule eye exams during pregnancy, as hormonal changes can worsen eye conditions.
8. How is diabetic eye disease treated?
There are several ways to treat diabetic eye disease, including:
- Laser therapy to seal leaky blood vessels
- Injections to reduce swelling
- Surgery to remove blood that fills the center of the eye or repair a detached retina
9. Can diabetic eye disease be prevented?
While there’s no guaranteed way to prevent it, actively managing your diabetes and having regular eye exams can greatly reduce your risk for damage to your eyes. The National Institute of Diabetes and Digestive and Kidney Diseases highlights the importance of early detection and control.
10. What should I do if I notice changes in my vision?
If you experience vision will be blurry, dark spots, or sudden loss of sight, seek immediate medical attention. Prompt care can help treat diabetic eye disease and prevent further damage.
By taking proactive steps today, you can protect my eyes and lower your risk for diabetic eye disease in the future.